What is AMR
Developed by Dr. Kayley McCubbin, DVM, MSc, PhD Candidate, University of Calgary
Antibiotics are a subset of the larger group of ‘antimicrobials’, which means ‘anti-microorganism’ and can refer to agents intended to kill or slow the growth of bacteria, viruses, fungi, or parasites. Antibiotics, in particular, either kill or slow the growth of bacteria, and are used across a wide range of sectors, such as human and animal medicine, agriculture, horticulture, and aquaculture.
Since the introduction and adoption of antibiotic use, bacteria have developed ways to survive antibiotics, and this is what we refer to as ‘antimicrobial resistance’. Due to their relatively short lifespan, bacteria can do this by developing genetic mutations that protect them against antibiotics. Mutations can be passed on to bacteria of the same species through reproduction or can even be transferred to bacteria of other species. Some bacteria may even naturally have special features that make it easier for them to resist antibiotics.
Problems arise when the bacteria become resistant to antibiotics that were previously effective. This means that antibiotics used to treat certain bacterial species may no longer work as intended, or not work at all. When bacteria become resistant to more than one antibiotic, this is called multidrug resistance (MDR), which can pose major problems for treatment. MDR bacteria are often referred to as ‘superbugs’; bacteria that result in untreatable infections.
Mention of ‘antimicrobial resistance’ (AMR) commonly includes reference to ‘superbugs’ and apocalyptic scenarios. While these associations seem dramatic, there is reason for global concern. AMR is already a pandemic causing a large number of deaths and is only increasing in severity. We first need to understand what it is, how it develops, and what considerations are essential for control, to fully recognize the extent of the issue.
Who is at Risk?

What are the Impacts?
Infections with resistant bacteria can cause increased illness severity and longer times to resolve the infection, or even result in death. If an infection is untreatable by antibiotics, organ failure can occur which significantly impacts quality of life or can be fatal. Bacterial infections of this nature are on the rise and are projected to increase, dramatically impacting human and animal populations in the coming years. Advances in health made due to antibiotics may no longer be possible. We may regress into a pre-antibiotic age, where bacterial infections are again a leading cause of death, globally.
What Causes AMR?
Antibiotic use contributes to the development of resistance by killing those bacteria that are susceptible and leaving those with the ability to prevent antibiotic action.
One of the main contributing factors to the development of resistance is antibiotic use, including overuse. While antibiotics are an important part of healthcare, agriculture, horticulture, and aquaculture, there are many circumstances where they are being misused.
Another contributor is improper antibiotic dosing even when antibiotics are required. Bacteria are exposed to antibiotic doses below a level that would kill or slow bacterial growth (sub-therapeutic), but instead, lead bacteria to develop resistant genetic mutations overtime. This may occur with the use of personal care or other products that we use every day (e.g. soap, cleaning agents) that are labeled as ‘antibacterial’. It is very important to use antibiotics only when needed and as directed by a clinician, to limit the development of resistance.

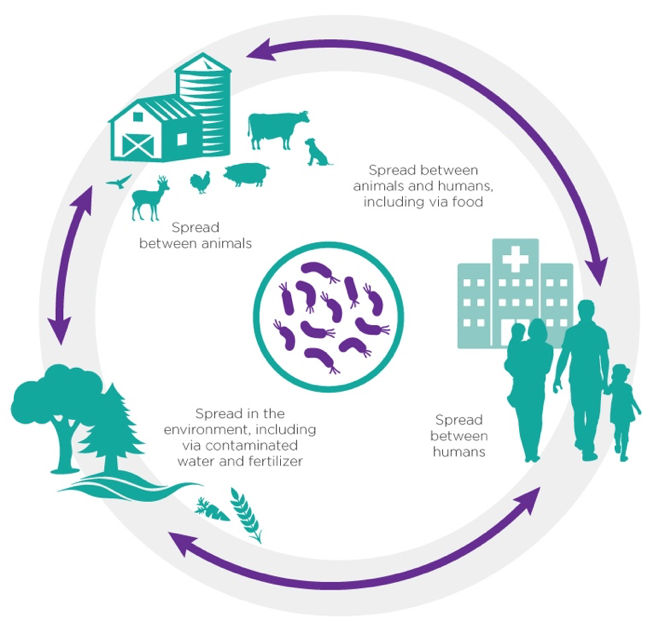
Why AMR is a One Health Issue
A “One Health” problem is one in which interactions between humans, animals, and environmental factors must be considered, and an approach encompassing all aspects is required to control and/or prevent the problem. For this reason, AMR is an example of a One Health issue.
As there are a limited number of antibiotics available for use, the same active ingredients are often used in antibiotic products intended for humans, animals, and agriculture. Not only can antimicrobial resistance arise due to use in humans or animals, but it can also develop in soil or water when antibiotics are used for aquaculture or crops.
When bacteria become resistant due to excessive antibiotic use in one sector or species, it can lead to serious health implications in other sectors or species. This is why a One Health approach, encompassing expertise and decision-making in all sectors impacted by antibiotic use is required.
Antimicrobial resistance is a global challenge that requires collaboration across many industries and health sectors. This is important to identify areas for intervention to limit the continued development of resistant bacteria for the benefit of humans, animals, and the environment alike. The AMR - One Health Consortium aims to facilitate such collaboration by acting as a Pan-Alberta platform for research, policy, training, and outreach in this area.
Additional Resources
International resources:
World Health Organization (2018, February 15) Antimicrobial Resistance: Key Facts. Retrieved from https://www.who.int/en/news-room/fact-sheets/detail/antimicrobial-resistance
Centres for Disease Control and Prevention (2019, November 4) Antibiotic/Antimicrobial Resistance (AR/AMR). Retrieved from https://www.cdc.gov/drugresistance/about.html
Canadian resources:
Becton, Dickson and Company (2018) The Truth About AMR in Canada. Retrieved from
https://www.national.ca/workspace/uploads/files/the-truth-about-amr-in-canada_nov18.pdf
Government of Canada (2018, November 16) Antibiotic (Antimicrobial Resistance). Retrieved from https://www.canada.ca/en/public-health/services/antibiotic-antimicrobial-resistance.html
National Collaborating Centre for Infectious Diseases (2019) Antimicrobial Use and Resistance. Retrieved from https://nccid.ca/collection/antimicrobial-resistance/
Council of Canadian Academies (2019, November 12) When Antibiotics Fail. Retrieved from https://cca-reports.ca/reports/the-potential-socio-economic-impacts-of-antimicrobial-resistance-in-canada/
Alberta resources:
Government of Alberta (2018, July 30) Drug Resistance or Antibiotic Resistance. Retrieved from
https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=std139567&lang=en-ca
Literature Cited
- O’Neill (2016, May) Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Retrieved from: https://amrreview.org/sites/default/files/16 0518_Final%20paper_with%20cover.pdf
- World Bank (2017) Drug Resistant Infections: A threat to our economic future. Retrieved from http://documents.worldbank.org/curated/en/3 23311493396993758/pdf/114679-REVISED-v2-Drug-Resistant-Infections-Final-Report.pdf
- Public Health Agency of Canada (2018, April 17) Canadian Context on Antimicrobial Resistance. Retrieved from: https://www.cadth.ca/sites/default/files/symp-2018/ presentations/april17-2018/Concurrent-Session-E6-Antimicrobial-Resistance-Drugs.pdf.